With thousands of deaths from coronavirus across Britain, we look at some of the Tamils healthcare workers the frontlines of the battle to save lives in the National Health Service (NHS).
From nurses and doctors to our paramedics and porters, every single contribution is invaluable. And alongside thousands of other workers, the Tamil community has been actively involved in efforts to fight the pandemic.
Throughout this month we will update the page to bring you testimonies from those on the frontline of the NHS.
Arun Kirupakaran, Doctor, London
"I was moved from my day job as an ophthalmology trainee doctor onto the medical covid rota, where I now work 12 hour day and night shifts. It was a huge change to what I was used to! Seeing patients on the ward feels like a lifetime ago. Now my job involves clerking in patients in A&E, reviewing their oxygen saturations, ordering chest X rays and having difficult conversations with patients and their relatives about the potential consequences of coronavirus."
"Patients vary vastly in terms of their age, past medical history, baseline functional status; not just 'typical elderly patients with co-morbidities' as classically presented in the media. The most common symptoms are fever, headache, dry cough, back pain and loss of smell. These are not the ONLY symptoms though. 10% of patients present with gastro-intestinal symptoms such as nausea and diarrhoea."
"Everyone is scared. Doctors, nurses, patients, relatives, the general public. No one was prepared for this pandemic. We will get through this together and be back to our daily routines soon. But until then we all have a duty to be nice and help each other. Support yourself, your family, friends, neighbours and work colleagues. Check up on all of them and try stay positive. Before we know it life will return to normal."
Thibyaa Mahasivam, Paediatric Intensive Care Nurse, London
Before going to nursing school you choose the field of nursing you want to study. I chose Paediatrics. I thought this meant was that I would never have to take care of an adult in my nursing career, ever. But then COVID came.
Like me, many others wondered what was going to happen in the world of paediatrics. This wasn’t stepping out of our comfort zone...this was LEAPING out of our comfort zone. All admission onto PICU (unless an emergency) was put on standstill. We started to prepare ourselves for the world of critically ill adults.
Not one of us hesitated to step forward when the biological war came knocking on the ward door. Yes many of us complained, we had every right to - this was how we were able to unload our stress and worries. But when given the choice to relocate elsewhere the vast majority of us chose to put our lives on the line.
In a matter of days, the Intensive Care Unit transformed to accommodate adults. Nurses went to AICU to learn the skills they needed. Countless emails flooded my mailbox telling me: how to resuscitate an intubated adult with coronavirus; what medications were commonly used in adults; what the ‘normal’ is; how to protect myself and keep myself safe before I treated the patient; the list continues. A multitude of simulation classes were put into place. There was so much information to be processed but the nurses continued. The speed at which these nurses adapted was phenomenal.
Taking care of an adult is very different to taking care of a child. But here I stand with my coworkers doing something I thought I’d never do.
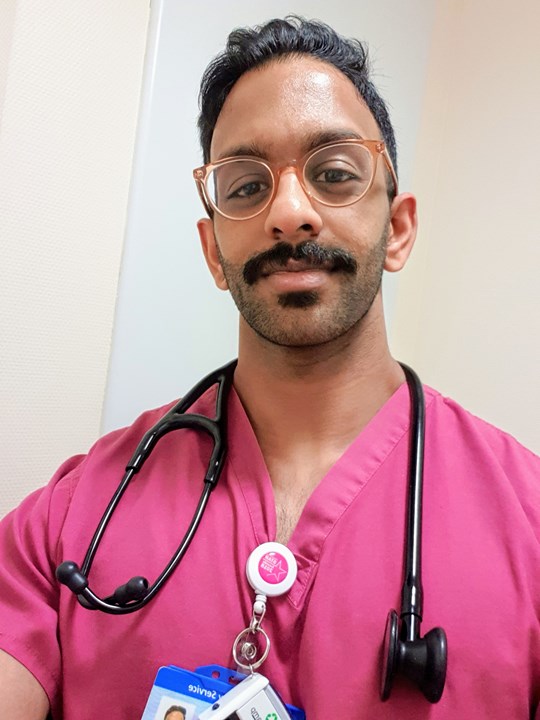
Ramanan Gukathasan Doctor, London
“The last few weeks have been daunting and demanding. We healthcare professionals (HCPs) and the wider community are facing something never before experienced; the importance of us working together to get through this cannot be stressed enough.
These are strange and scary times, both inside the hospital and the outside world. I have had to get used to a whole new way of working when treating “Covid-suspected” patients and my rota has been upheaved to ensure the hospital is better staffed through day and night. This is going to be a marathon, not a sprint.
Working on the so-called “front-line”, I have seen how quickly people can deteriorate with Covid-19. People may think HCPs are the only one who can do anything about this; however, that is not the case. We, the HCPs, are not your front-liners anymore; we are your last line of defence. You, the public, are the front-liners now.
The public have a vastly important role to play in all of this by practising social distancing. It is the strongest (and possibly only) tool we have to take control of this situation and stop it in its tracks.
Only go out when you need to. Stay at home unless it is absolutely essential i.e. going to the shops, to work or to hospital for a genuine emergency. As someone who is passionate about health & fitness, I advise you to get some degree of daily exercise and sun exposure (I understand this may be difficult depending on where you live!). Direct exposure to sunlight is your best source of Vitamin D, which is linked with a healthy immune system. Exercise stimulates endorphin production which also plays a role in the immune system and contributes towards a positive mindset. If you have access to a garden and fitness equipment at home, use it; make sure you avoid crowded areas if you need to go outside your house for exercise.
In addition to all of these, aim to:
- Eat well.
- Sleep well.
- Drink plenty (of water!).
- If you smoke, try to cut down or give up - you will need your lungs.
- Focus on your mental health - if it means having a drink every now and then that is okay, but try to avoid using junk food, drugs or alcohol as coping mechanisms for stress or boredom; meditation is a helpful tool.
- Stay in touch with friends and family regularly through technology.
- Check in on your neighbours, especially if they’re elderly.
- Don’t watch the news all the time; it can be overwhelming.
- Develop a hobby/interest, maybe learn a language.
But most of all, stay positive. We will get through this, together. Stay at home and stay safe.”

Niro Kuganenderan, Doctor, London
Today is my first day off in a while. Whilst I am sitting here reflecting on my week, there was one day last week that I found particularly hard.
3.30 pm. I was on-call. I was just about to sit down to have a bite to eat. The surgery was busy with over a 100 phone calls that morning. Another call came in. Reception called me to say, Niro you better take this. On the line was one of my patient’s wife. She rings to say that she thinks her husband has just died but she couldn’t be sure. She says please can you come? He had COVID-19.
A few thoughts went through my head, do I go and see him? The new Coronavirus Act means a competent family member can verify death, shall I just get the wife to do it? No that can’t be right, I better not to do that. Shall I video-call the wife? Or just get the district nurses to go who were visiting him in a few hours anyway? After a few wrestling thoughts , I decided the right thing to do was to go myself in some basic PPE.
When I got to the house, the wife was by her husband’s bedside, holding his hand. I knew when I looked at him. I said I am so sorry. She just burst out crying. His children, all grown up and live away were waiting outside all gathered in the garden, 2m apart. I had to break the news. Everyone started crying. My tears couldn’t hide behind my visor.
But you know what the hardest part was? Due to Covid-19 and household isolation they couldn’t even come into their beloved family home.
They couldn’t even give their mum a hug. They couldn’t see their dad’s face for one last time. They couldn’t touch their dad’s hand for one last time. They couldn’t even say goodbye.
We clap for our key workers who are all doing a fantastic job in difficult circumstances BUT we must remember the people who have been affected by Covid-19. Next time we clap for our carers, let’s spare a thought for all the people who are dying on their own with no family around them. We cannot forget the grief of the families who have lost their loved one and have been robbed of one of the most basic human rights- the ability to grieve.
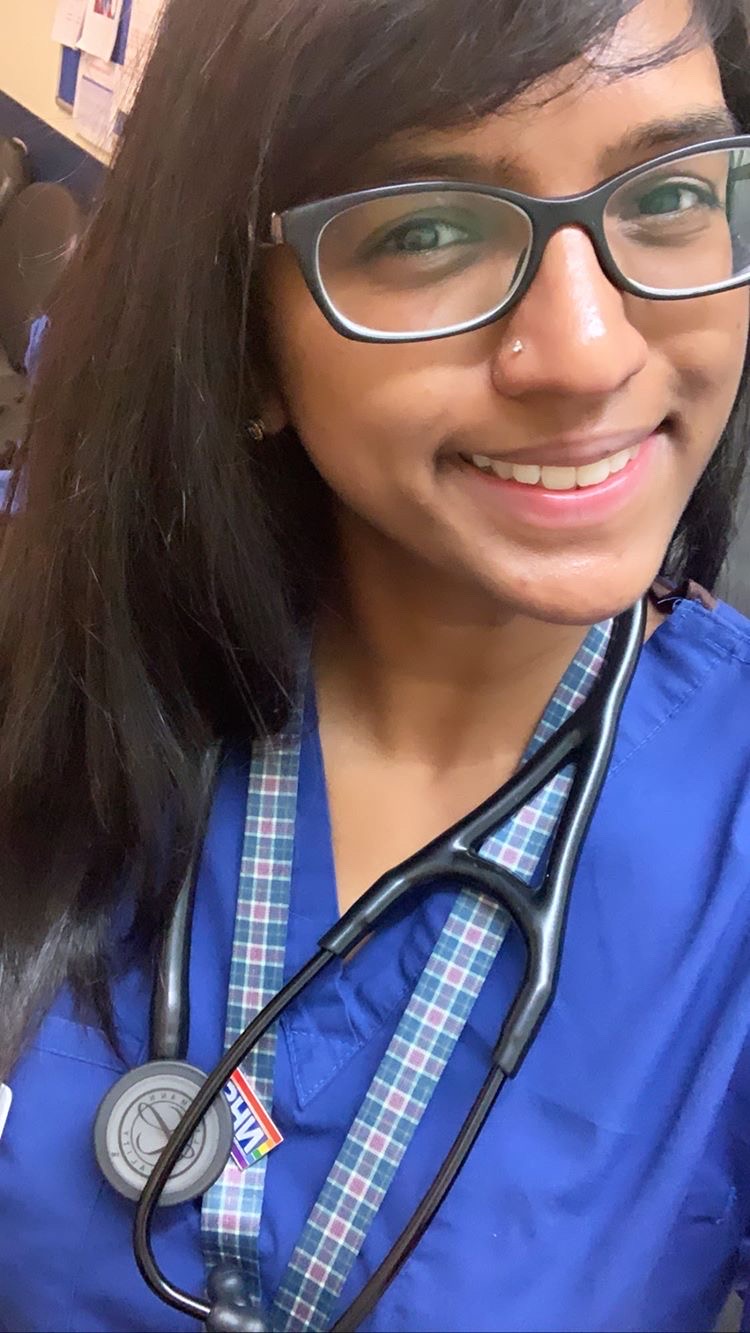
Agalya Ramanathan, Doctor, London
I am a junior doctor working in a busy London hospital. We had our first few cases of coronavirus nearly a couple of months ago, and it is now taking up many wards throughout the hospital. As a result, doctors have had to change their working patterns with limited notice to join a special coronavirus rota. This includes doctors who do not normally work on medical wards such as ophthalmologists and dermatologists. This has been designed to mobilise more staff so there are more doctors available to look after these patients, whilst accounting for sickness amongst staff members.
I have seen patients who are affected by coronavirus in different ways, including patients who are very sick and have been moved to intensive care. I have also seen patients who have returned to normal wards post intensive care and been discharged, as well as patients who only had minor symptoms and were admitted for other reasons. Unfortunately I have also seen patients, or heard of patients, who have required intensive care but who either were not candidates for this (due to other illnesses) or could not go there due to a lack of capacity. The hospital is working to increase beds and staffing so that we can have more ventilated beds to look after these very sick patients but it is not clear if this will be enough. It is difficult to look after these patients as there are no curative treatments. It is a new virus and although experimental treatments may be tried in certain places, the evidence is limited. As a result there is a lot of staff anxiety as well.
My message to anyone reading this would be to take coronavirus seriously, to look after yourselves and families and to take sensible measures to avoid spreading infection. Young healthy people tend to only get mild symptoms but others are not as lucky so please be considerate and follow the social distancing guidance.

Meenakshi Bala, Doctor, Birmingham
I’m in my second year of being a doctor so it’s been a huge change to a work-life I was just getting used to. Working on a respiratory ward in the biggest trust in the country we were one of the earliest to get hit by COVID-19. More than half my team have been off sick at some point with one of them being treated as an inpatient.
I’m generally an emotional person and I think it makes me better at my job, however, this has been unbearable at times. During our first week on our new rota which consists exclusively of 12.5hr shifts, a doctor who has over 8 years more experience told me frankly, “I’m not coping emotionally with this.” The medicine is straightforward supportive care which offers little room for us to improve outcomes, patients spend most of their time alone since visitors aren’t allowed and I’ve had countless conversations over the phone to tell families their loved one is deteriorating or has passed away.
It is undeniably a difficult time for everyone which is why more than ever it’s crucial to support each other as a community and society in the ways that we are able to. That looks like showing gratitude and practical help to our essential workers, preventing the spread of fake news, keeping in touch with loved ones virtually and ensuring we do what we can to keep ourselves healthy.
When we all act as a community we not only limit the spread of this virus but also help each other get through its consequences.
Thuvaraga Arulampalam, Doctor, London
"2020 has become an extremely hard time for all of us, probably one of the most testing times for some. I love my job in Intensive Care but nothing has prepared us for this. Patients are dying without their loved ones; they are being held by strangers in plastic and the last voice they hear is unfamiliar. I never thought my job would be a reason for me to stay away from all of my loved ones. Inpatients are being tested positive for the virus 10 days later because of spread from visitors who thought they were safe because they didn’t have symptoms. We’re shutting down bays because now all of the patients may have it."
"My nursing colleagues are anxious because they are returning home to their children, their loved ones with chronic diseases. A few days ago, my boss cleaned the floor of our covid-unit because our cleaning staff had not been tested for PPE yet. He’s worked 12 hours every day for two weeks because his colleagues had to self-isolate. We’re all finishing our 13-hour shifts and returning home to read and learn more so that we are prepared for the next patient. I’m working with some brilliant anaesthetic consultants who are having to up-skill and work 90 hour weeks. My heart is heavy, however, I’m grateful to be able to go to work and be alongside some amazing colleagues. It upsets me that on my way to work, I see so many people walking around in groups."
"As a race we’ve seen and been through tragedy and trauma, we can get through this."
"My plea from the bottom of my heart - Stay away from your loved ones now so you have a chance to see them soon. We stay at work for you, please stay at home for us."

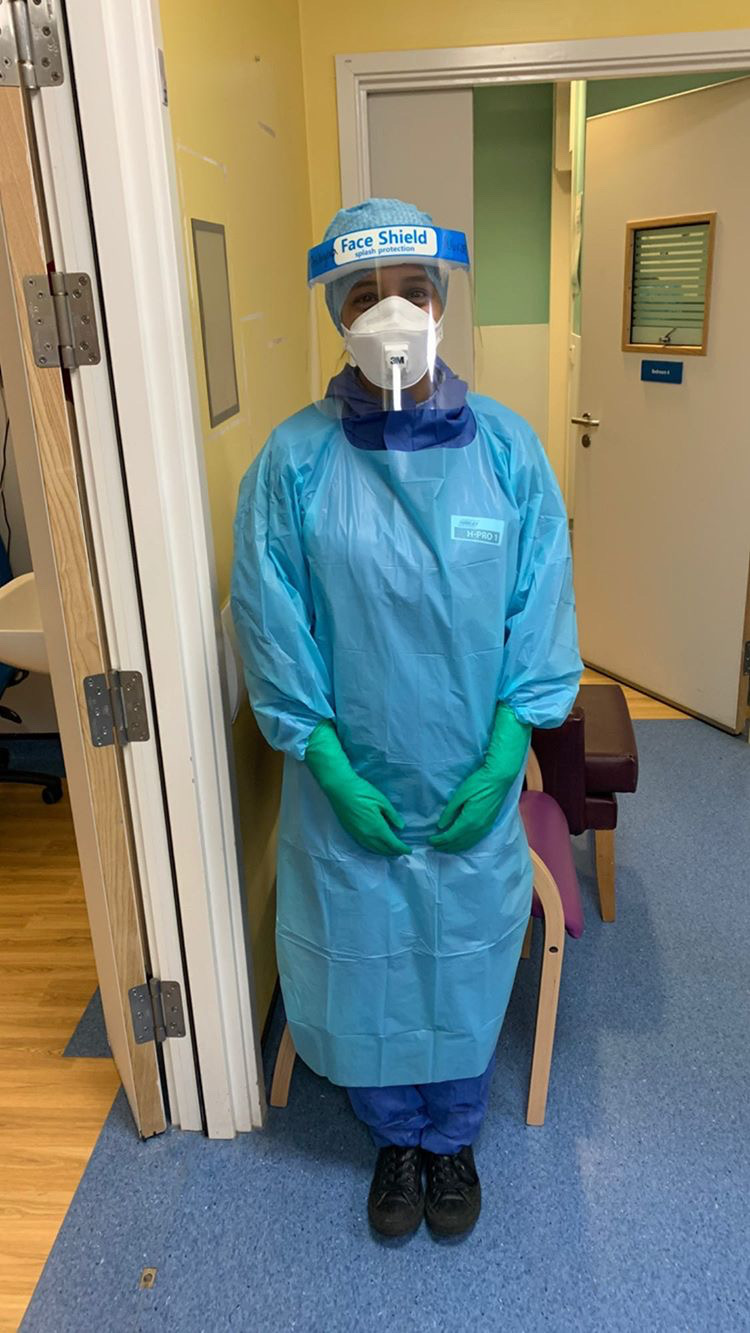
Tharani Pathmarajah, Rapid response practitioner, London
My primary role is to assess acutely unwell patients in the community who are identified as at risk of hospital admission. Being a physiotherapist by background, I also support patient discharges from hospital to home. These services are essential to the current covid-19 pandemic as we are increasingly identifying and treating COVID positive patients. Our service also helps with ensuring that beds made available in hospital for these patients and rehabilitating them at home. Community services in general provide a vital part of the network between GP’s, hospitals and adult social care and I find my role very fulfilling.
Ashmi Ganeshamoorthy, Doctor, London
“From a personal experience, the last couple of weeks have been challenging and tiring. Aside from getting used to completely new ways of working, there are many psychological challenges. As junior doctors we are very much at the frontline with COVID patients and due to shortage of Personal Protective Equipment (PPE), we are not being given adequate protection. Seeing our colleagues having to self isolate one by one only adds to the pressure.”
"There have been times where we had to see patients (whom COVID status were unknown) without any PPE, and the next day same patients developing symptoms and testing positive for COVID."
All the above will only cause anxiety for a limited amount of time. But after that you reach a point where you learn to accept it and get on with your work. It has not been easy for our family and our loved ones.”

Gaya Mahalingam, Doctor, Luton
“I'm a Foundation Year 2 trainee working in Accident & Emergency for the last 4 months and also during these difficult times tackling COVID-19.
It's been a mixed bag of emotions working on the front line and I've witnessed things I didn't think I would so early on in my training. This is no joke, witnessing people with severe symptoms, needing ITU support and struggling with breathing symptoms ; and all done by themselves because this isn’t an illness where you can be by your loved ones side; that's probably one of the hardest things to witness.
Please don't think this won't affect you, by going out and visiting family you are putting people at risk. Please wash your hands. Please stay indoors. Please help us. “
Mayuri Jeganathan, Optometrist, London
“I was still going into work to provide primary eye care for patients who have emergency or essential eye problems. That would for example include a key worker who has broken their glasses and requires them to continue work. Or a patient who has suddenly started experiencing pain in the eyes and needs immediate care. Essentially, to be able to help people of the general public to allow them to continue working or to keep them out of a hospital as far as necessary.
It has been an interesting shift in my work pattern as usually work is quite busy for me, but in amongst this, it has been humbling to know that everyone is looking out for each other and keeping best interests at heart. More than anything, if I didn’t appreciate the NHS and its workers enough, from porters to HCPs, I now appreciate them and their hard work even more.
Shout out to every single other worker out there (waste collectors, supermarket workers, policemen and shop owners) including both my parents, who are staying open to continue providing essential goods and services to their local communities! We salute you."